The Covid-19 pandemic has not impacted all ethnicities equally in the UK: as early as three months into the first wave, evidence was mounting that non-White British were much more likely to be hospitalised, and more than two times more likely to die, of Covid-19 than the white British majority once age and geographical factors were taken into account.
Updated estimates at the end of the summer found the disadvantage had continued, and the Government continues to acknowledge the greater severity and mortality among minority groups in the UK, linking these risks to variation in the demographic, socioeconomic, and underlying health vulnerabilities across different ethnic groups.
While socio-demographic factors explain some of the differences in Covid-19 impact across ethnic groups, substantial inequality remains even after occupation, household structure, age, sex, income geography and poverty are taken into account. One – as yet unexplored – mechanism that may underlie ethnic differences in Covid-19 impact is health behaviours practiced by individuals themselves. If different ethnic groups have different levels of adherence to recommendations such as hand washing, mask wearing, or maintaining social distance, this might explain some of the inequality we observe in Covid-19 impact.
Ethnic differences in health behaviours are well-documented in the UK, with marked variation in terms of substance use, diet, and physical activity. To explain this variation, social scientists point towards a number of underlying differences, most notably differences in the opportunities and costs of health behaviours arising from socioeconomic ethnic inequality and the risk of discrimination and harassment in the local or medical community. Increasingly scholars also explore the role of ethnically structured social norms, for instance documenting how variation in health behaviours can be attributed to social norms prevalent in their co-ethnic community or, in the case of immigrants and their descendants, in their country of origin.
Using data from a one-of-a-kind survey of recent University graduates from the UK, MiSoC researchers Angus Holford, Renee Luthra and Adeline Delavande provide new evidence on the role of socioeconomic and demographic factors as well as the strength of ethnic ties in determining adherence to recommended health behaviours during the pandemic. This paper moreover includes novel measures of ethnic differences in the perceived risk and expected severity of Covid-19 transmission, as well as the perceived efficacy of health behaviours in mitigating this risk. We show that despite the fact that ethnic inequalities in Covid-19 prevalence and severity were well-publicized, ethnic minority young adults did not report substantially different subjective expectations about the virus than the White British minority. Therefore, different perceived risks do not explain their higher adherence to public health guidelines. Nor does their (higher) objective risk due to public transportation use, working conditions, or housing conditions. Rather, ethnic differences are most pronounced among those minorities who are most strongly embedded in a co-ethnic peer network, and among those who have higher levels of trust in state intervention. These findings point towards the importance of harnessing ethnic communication and influence channels to ensure adherence to public health policy in the UK.
Our Question: Are there ethnic differences in adherence to recommended health behaviours related to Covid-19?
To examine this question, we use a unique dataset that includes detailed data on Covid-19 related health behaviours for an ethnically diverse sample of recent university graduates aged between 22 and 25. This data, part of the larger BOOST project, was collected from a sample of recent University graduates via a web survey on June 12-July 3, 2020 at the end of the first major lockdown in the UK, shortly before restrictions were eased. These survey respondents had already participated in 4 years of data collection prior to the pandemic, during which a wide array of information on their social class background, school performance, and friendship networks was gathered. Particularly important for this project, the survey also elicited the subjective expectations of the survey participants regarding their risk of contracting Covid-19, their expected severity of sickness should they contract it, as well as their perceived efficacy of different health behaviours that were officially recommended at the time: hand washing, mask wearing, social distancing, and avoiding non-essential outings and public transport. The data is not representative of all young people in the UK, and comparisons between our sample with data from the Higher Educational Statistics Agency data and University administrative records show that we surveyed more women, ethnic minorities, and higher performing recent graduates than the average. Still, this data is one of a kind, allowing us to answer not only whether there are ethnic differences in Covid-19 related health behaviours but also why this might be the case.
Ethnic Differences in Covid-19 Related Health Behaviours
In Panel A we report the percentage of our sample who report never engaging in activities which increase the risk of contracting Covid-19: exercising outside of the home, visiting relatives from outside your household, attending a gathering of more than 3 friends outside of the household, going shopping for groceries or essential items, shopping for non-essential items, and traveling on public transport.
Fairly consistently across these measures, both Black British and White Non-British (mostly European) young adults in our sample are more likely to avoid activities which increased exposure, with the one exception of more frequently taking public transportation.
Asian British young adults were also more likely than White British to avoid exercise and shopping for non-essential items, but were more likely to visit relatives and similarly likely to gather in larger groups of friends, as well as travel on public transport.
Panel A: Outside exposure, percent “Never”
| How often in the last week have you done the following things? | White British | Black British | Asian British | White Non-British |
|---|---|---|---|---|
| Exercised outside your home | 15 | 25 | 26 | 27 |
| Visited relatives from outside your household | 55 | 61 | 51 | 73 |
| Attended a gathering with more than 3 friends from outside your household | 64 | 68 | 63 | 67 |
| Gone out shopping for groceries or essential items | 11 | 13 | 16 | 12 |
| Gone out shopping for non-essential items | 48 | 57 | 56 | 52 |
| Travelled on public transport | 86 | 66 | 79 | 73 |
| N | 628 |
In Panel B we show ethnic differences in our sample in the percentage reporting always practicing social distancing and hygiene practices recommended to reduce the risk of contracting or transmitting Covid-19. In terms of washing hands or wearing a face mask in public, all ethnic minority groups are more likely to report always practicing these measures than White British. For social distancing 2 meters in public, the evidence is more mixed, with white British more likely to social distance than Black British and Asian British, but less likely than White Non-British.
Panel B: Social distancing and hygiene practices, percent “Always”
| Over the past week, how much of the time have you done the following things? | White British | Black British | Asian British | White Non-British |
|---|---|---|---|---|
| Worn a mask or face covering outside the home | 9 | 25 | 20 | 21 |
| Social distance 2 m in public | 62 | 56 | 47 | 71 |
| Washed your hands as soon as you get home | 73 | 82 | 89 | 86 |
| N | 628 |
In general, ethnic minority young adults in our sample are more likely to adhere to recommended Covid-19 related health behaviours than White British young adults.
Explaining Ethnic Difference in Covid-19 Health Behaviours: Risk Factors
Having observed ethnic differences in Covid-19 health behaviours, we next sought to explain them. We know from the existing literature that ethnic minorities differ from the White British majority in many ways that might explain why they behave differently in relation to Covid-19. Some differences, such as their age profile and education levels, are already held constant in our study because our sample contains only young adults who are university graduates. However, we also examined how the results above changed once we took into account several other potential explanations:
1) Socio-economic background: It is possible that young people from more affluent backgrounds might be able to socially isolate at home more comfortably, for instance, or that young people with particularly high levels of academic performance or a degree in a STEM subject might be particularly likely to respect official public health guidance. Given well documented ethnic differences in economic well-being and academic performance, we therefore adjusted for differences across the groups in terms of whether their parent had a degree, whether they had obtained a first degree classification, and whether their degree was in a STEM subject.
2) Living situation: We know, for instance, that Asian minority groups are more likely to reside in multi-generational households, where young people may be seeking to shield elderly family members; we also know that White British are more likely to live in rural areas with less access to public transport and more space to social distance when outdoors. We therefore also adjusted for whether the young people in our sample lived in their own household, with their family, or in a room in a shared household, and whether they resided in an urban area, near a large city or town, or in a rural location.
3) Finally, the concentration of ethnic minorities in high risk occupations including healthcare and delivery services has also received a great deal of scholarly and media attention. We therefore control for whether the sample member was working in their usual workplace in a higher risk occupation (defined as those working in health, teaching, caring, sales and customer services), at their usual workplace in a lower risk occupation, or whether they were not currently working or working from home.
In general, and contrary to our expectations, many of these factors were not consistently related to health behaviours. Few differences emerged, with the exception that women were more cautious (less likely to gather socially, more likely to social distance in public, and more likely to wash hands), and those who lived in suburban areas engaged in more risky behaviours (more likely to gather socially, and less likely to social distance than those living in rural areas). Public transport was perhaps the most socially patterned behaviour: not surprisingly, those living in urban and suburban areas, living away from families, and working away from their home were much more likely to use public transport.
For most of the health behaviours studied here, ethnicity remained a source of difference even holding constant socio-demographic, living situation, and work characteristics. With some variation, White British adults adhered less to recommended Covid-19 health behaviours than minority groups. As compared to White British, all other groups were less likely to exercise outdoors and more likely to wear a mask. White Non-British remained less likely to visit family members outside their household, Black British were less likely to shop for non-essentials, and both Asian and White Non-British were also more likely to wash their hands.
In contrast, controlling for ethnic differences in socioeconomic background, living situation and working lives, there was no remaining ethnic differences in the likelihood of gathering with friends or shopping for essential items, and Asian British were less likely to always social distance, and Black British more likely to use public transport.
Explaining Ethnic Difference in Covid-19 Health Behaviours: Subjective Expectations
Given that ethnic differences in social background, living situation and working lives do not explain inequalities in Covid-19 health behaviours, we next turned to differences in subjective expectations as a possible source of ethnic difference.
The differential impact of Covid-19 by ethnicity, in terms of both the likelihood of contracting the virus and its severity, was already well publicised at the time our survey launched in mid-June 2020. We therefore surmised that differences in adherence to recommended Covid-19 related health behaviours is a rational response to higher levels of perceived risk among ethnic minority groups.
To test this hypothesis, we elicited the subjective expectations and attitudes of survey respondents. Respondents were asked to rate the maximum and minimum probability, on a 100 point scale, of the likelihood that they would die if they contracted Covid-19 and the likelihood they would be hospitalised if they contracted Covid-19. This measure enabled us to take into account not only different perceptions of the severity of Covid-19, but also different levels of uncertainty in assessing the potential severity. We also asked respondents to rate the likelihood of contracting Covid-19 under two scenarios: a high risk scenario, where they visited family members and friends outside their household every day, used public transport and went shopping every day, and never wore a mask, and a low risk scenario, where they never visited family members or friends outside their household, only went shopping once per week, never used public transport and always wore a mask. The difference between the two scenarios was computed and displayed below as the perceived efficacy of safe behaviours. Finally, we asked respondents about their preference for state income redistribution in a battery of 5 questions, on a 7-point scale, and used the average as a proxy for trust in government in general.
As can be seen in Panel C below, there is only very small differences in the subjective expectations of Covid-19 severity among our sample members by ethnicity, and only Black British differ from White British in their perceived efficacy of health behaviours. Both Black British and Asian British show a higher preference for redistribution, a proxy for trust which might explain their higher adherence to public health guidelines.
Panel C: Subjective Expectation of Severity of Covid-19, Efficacy of Safe Behaviours, and Preference for Redistribution
| Average estimated… | White British | Black British | Asian British | White Non-British |
|---|---|---|---|---|
| Max Probability of Death | 20.43 | 21.86 | 23.51 | 14.49 |
| Min Probability of Death | 6.12 | 8.51 | 7.90 | 4.15 |
| Max Probability of Hospitalisation | 34.33 | 30.67 | 32.61 | 28.59 |
| Min Probability of Hospitalisation | 11.27 | 13.35 | 13.26 | 10.09 |
| Perceived Efficacy of Safe Behaviours | 36.94 | 31.26 | 36.14 | 37.18 |
| Preference for Redistribution (proxy: Distrust of government, progressive attitudes) | 4.59 | 4.98 | 4.81 | 4.39 |
Given the surprisingly minor ethnic differences in attitudes and expectations, we did not anticipate that controlling for these factors would alter the ethnic differences in health behaviours described above, and indeed ethnic differences remained largely unchanged in subsequent models where they were included.
Explaining Ethnic Difference in Covid-19 Health Behaviours: Ethnic Norms
A final explanation for ethnic differences in Covid-19 related health behaviours may be norms that are specific to minority communities. These norms may be general, such as stronger preferences for state intervention which may prompt greater adherence to public health guidelines, or they may be specific to the health behaviours themselves, for instance culturally patterned norms of handwashing, wearing face coverings, or maintaining social distance in public settings. Previous research has found, for instance, that immigrants tend to import social norms around smoking and alcohol consumption from their sending countries, which helps explain why South Asian women smoke less, and South Asian men and women drink less, than their White British counterparts. These culturally specific health behaviours are generally stronger among ethnic minorities with higher levels of ethnic attachment, in other words who reside in areas of higher ethnic minority concentration, who have a friendship network comprised of a higher proportion of people of their same ethnicity, or who profess a stronger ethnic identity.
The fact that we cannot explain ethnic differences in health behaviour adherence even with an extensive set of sociodemographic controls, as well as our very unique measures of subjective expectations, suggests that unobserved ethnic norms surrounding Covid-19 related health behaviours may underlie the remaining difference. While we have no direct measures of such norms, we can triangulate information on ethnic attachment to test whether adherence to recommended Covid-19 related behaviours is stronger among those who are more likely to be exposed to ethnic minority norms. To do so, we examine how ethnic differences in health behaviours vary among those with a higher and lower proportion of close friends of the same ethnicity.
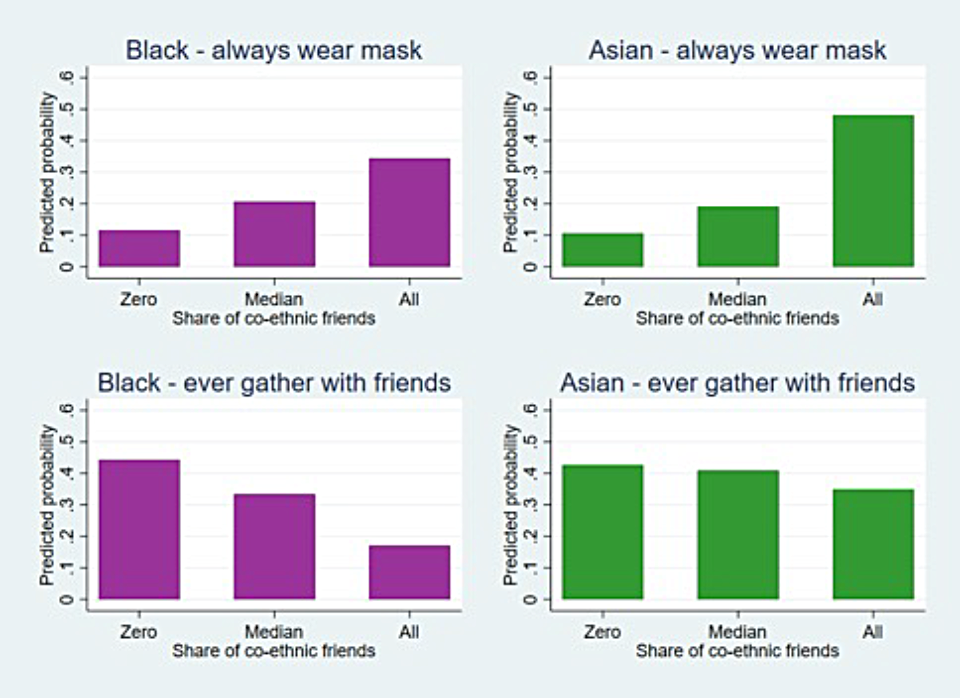
In the Figure below, we illustrate the relationship between ethnicity, friendship network composition, and health behaviours for both hand washing and gathering with friends. It is clear that ethnic minority young adults with a higher proportion of same-ethnicity friends show stronger levels of adherence to many recommended health behaviours than those who were less attached to their co-ethnic community in University. There is not space to illustrate all these differences here, but Black British minorities with a higher proportion of co-ethnic friendships are less likely to exercise outdoors, less likely to visit relatives outside of their household, less likely to gather with friends, and more likely to wear a mask than those with a more mixed friendship network. Similar results are found for Asian British, who are statistically significantly more likely to wear a mask when they have a higher proportion of co-ethnic friends, as well as less likely to exercise, to visit relatives, and to gather with friends (though these differences are not statistically significant). The only Covid-19 related health behaviour with consistently lower adherence among minorities with stronger ethnic attachment is using public transport, though here the differences were not statistically significant.
Conclusion
Using a novel data source gathered during the first Covid-19 lockdown in the UK, MiSoC researchers were able to demonstrate marked ethnic differences in Covid-19 related health behaviours among an ethnically diverse group of recent university graduates. Against expectations, the researchers found that these ethnic differences were not explained by differences in perceived risk of Covid-19 or health behaviour efficacy, but rather were strongest amongst minority group members with more ethnically homogeneous friendship networks.
These findings provide further evidence of the ethnic embeddedness of health behaviours and the potential health benefits of ethnic attachment. Minority group members with a higher proportion of minority ethnic friends observed health behaviours that were more protective against Covid-19. This research also shows that health behaviours are responsive to risks, as those who perceived greater risk to themselves were more likely to distance, wear masks, and wash hands, and those who perceived greater risks of transmission to others reported less social interaction. However, ethnically structured social norms are certainly also important, and collecting data on people’s beliefs from ethnically diverse samples is necessary both for targeting public health messages and assessing how successful they have been.